This is a superb article reprinted from Life Extension Magazine and contains critical information that your doctor does NOT know... Dr Robin Willcourt
The Testosterone Controversy
By William Faloon
Testosterone levels are high in young men, but plummet during aging.
Despite compelling findings of efficacy, conventional doctors still question the value of testosterone replacement in maturing men. This oversight is causing needless heart attacks and strokes.
Low testosterone is associated with excess abdominal fat,1-4 loss of insulin sensitivity,5,6 and atherosclerosis.7,8
A critically important role of testosterone is to enable HDL to remove excess cholesterol from the arterial wall and transport it to the liver for disposal. This effect of enhancing HDL is termed “reverse cholesterol transport” and is vital to preventing arterial occlusion.9,10
Cardiologists routinely prescribe statin drugs to lower LDL, a lipoprotein that transports cholesterol from the liver to the arteries. These same doctors, however, fail to maintain sufficient testosterone levels in their patients to enable HDL to remove cholesterol buildup in the arteries. This is one reason why statin drugs have not always been shown to work in older men, who require functional HDL to keep arterial linings free of excess cholesterol. 11,12
Numerous studies document the vital role that testosterone plays in maintaining youthful metabolic processes throughout the body.6,7,13-21 A large new study confirms the deadly impact of low testosterone in older men.22
What’s scary are clinical trials designed by doctors who have no idea how to achieve youthful hormone levels. Men who enroll in these studies are subjected to lethal dangers because testosterone and estrogen blood levels are not properly balanced.
Cells throughout a man’s body are laden with receptor sites that are activated by the hormone testosterone. When testosterone is available to bind to these receptor sites, good things happen such as elevated mood and improved cognition in response to plentiful testosterone being available to the brain.23-25
Be it muscle, bone, vascular, or nerve tissue, testosterone provides critical command signals for your cells to behave in a youthful manner.8,26-33 As testosterone levels diminish, degenerative processes set in.
New Published Study Confirms Testosterone’s Benefits
Of considerable interest is the relationship between testosterone blood levels and cardiovascular events such as heart attack and stroke. In a revealing new study, researchers identified 2,416 men (aged 69-81 years) who were not on any kind of testosterone- affecting treatment. These men were subjected to a battery of blood tests that included total testosterone and estradiol (estrogen).
The first observation was that men with increasing levels of testosterone had a decreased prevalence of diabetes, hypertension, and body fat mass. Compared to men with the highest testosterone levels, those with low testosterone were twice as likely to have a history of cardiovascular disease. It was also observed that men with the highest testosterone levels were the most physically active.17
This large group of men was followed for an average of 5.1 years. Men in the highest quartile of total testosterone (above 550 ng/dL) had a 30% lower risk of cardiovascular events. Any level of total testosterone below 550 ng/dL resulted in significant increased risk, thus helping to establish a minimal baseline as to where total testosterone should be to guard against heart attack or stroke.
Estradiol levels measured in this group appeared to be mostly in safe ranges and did not impact incidence of cardiovascular events.
Data was tabulated based on hospital reports and/or death certificates for heart attack, stroke, unstable angina, bypass surgery, or stenting.
The four quartiles of total testosterone in this large group of older men were:
Quartile 1: Total testosterone below 340 ng/dL. (< 10 nmol/L)
Quartile 2: Total testosterone be-tween 341-438 ng/dL. (10 to 13 nmol/L)
Quartile 3: Total testosterone be-tween 439-549 ng/dL (13 to 17 nmol/L).
Quartile 4: Total testosterone above 550 ng/dL (> 17 nmol/L)
Of interest was the finding that Quartiles 1, 2, and 3 had about the same risk of cardiac adverse events. It was only in Quartile 4 (when total testosterone exceeded 550 ng/dL) that the 30% reduction in cardiovascular events occurred.
This finding showed that it did not matter if these men’s total testosterone was very low (below 340 ng/dL) or moderately low (up to 549 ng/dL)…they all had a similar increased risk for suffering a cardiovascular event. Only when total testosterone exceeded 550 ng/dL did cardiovascular risk plummet.
This finding remained consistent for cerebrovascular disease incidence, where men with the highest total testosterone (Quartile 4) had a 24% reduced risk of transient ischemic attack or full-blown stroke. The researchers noted this association with reduced cerebrovascular risk remained after adjustment for traditional risk factors.
The conclusions by the researchers who conducted this study were:
“Higher serum testosterone levels are associated with a reduced risk of fatal and non-fatal cardiovascular events in community dwelling elderly men.” 17
Mainstream Doctors Know Nothing About Hormone Balance
If you ever wonder why so many deaths are directly caused by medical errors, look no further than the obvious mistakes made by doctors who design human clinical trials.34-36
It has long been known that aging men are at risk for having excess activity of an enzyme called aromatase. The effect of surplus aromatase is that too much testosterone is converted to estrogen.37,38
Aging men have a propensity to develop dangerously high levels of estrogen combined with woefully inadequate testosterone, though many aging men suffer both low testosterone and estrogen.39,40
Elevated estrogen can sharply increase heart attack risk by promoting platelet aggregation and coagulation in coronary arteries.41,42 Higher estrogen in men also increases inflammation which can cause unstable plaque to rupture and occlude a coronary artery, thus creating a sudden heart attack.43-45
Now just imagine designing a study where a huge dose of testosterone cream is applied to dilapidated men with a high prevalence of obesity, hypertension, diabetes, and elevated LDL. These men (average age 74) all suffered limited mobility and many had known cardiovascular disease. All these physically impaired men had very low total testosterone levels (mean 243 ng/dL) at baseline, but the doctors never bothered to check their estrogen levels.
The study was stopped after six to twelve months because the decrepit men receiving testosterone (at a dose more than twice what is typically prescribed) showed a 4.6-fold increase in adverse cardiovascular events.46
The purpose of the study was to see if high-dose testosterone cream could improve strength and mobility in these degenerated men. Early results showed it to be effective in improving muscle strength, but the study had to be stopped because too many cardiovascular events occurred.
The study authors admitted that the testosterone cream may have converted to estrogen and caused these cardiac problems. My question is why they failed to test estrogen levels in the beginning and monitor estrogen after administering high-dose testosterone cream?
Obesity alone causes estrogen levels in men to spike.38 The reason overweight men grow breasts is that abdominal fat tissue synthesizes huge amounts of aromatase, which converts their testosterone to estrogen. Obese men with elevated estradiol are strongly advised to take aromatase-inhibiting agents.
By applying high doses of testosterone cream, estrogen levels would be expected to spiral upward in many of these unhealthy men, thus predisposing them to cardiovascular events inflicted by abnormal arterial blood clotting (thrombosis) and inflammation.
Despite these obvious flaws, this negative study was widely circulated in the medical mainstream and used as a basis to advice doctors to prescribe testosterone cream with caution.
This is unfortunate as the preponderance of data shows significant protective effects when testosterone and estrogen are in a youthful state of balance. Most published studies fail to look at estrogen levels in men, despite a massive body of evidence showing significant increases in mortality when estrogen levels are too high or too low.47-52
WHY TESTOSTERONE STUDIES ARE NOT CONSISTENT
One might wonder how two studies could come to completely opposite conclusions.
A 2011 published study of 2,416 men showed a 30% reduction in cardiovascular events when total testosterone levels exceeded 550 ng/dL.19
Yet an unpublished report released in 2010 of less than 700 men stated that cardiovascular events more than doubled when total testosterone exceeded 495 ng/dL.53
One problem relates to differing laboratory methodologies whose results vary more than professionals like to admit. This means that some of these studies may not have accurately measured testosterone blood levels. In the most recent positive study showing a 30% reduction in cardiovascular events in men with total testosterone above 550 ng/dL, the researchers exclusively used a mass spectrometry-based technique that provides a more accurate assessment of testosterone status than testing methods used in previous studies.
The more obvious flaw, however, relates to the large number of independent risk factors involved in the development of atherosclerosis, thrombosis and subsequent heart attack and stroke. While some of these other risk factors are sometimes factored in, no study on testosterone has included all of them and they all rely on outdated reference ranges for artery-damaging factors such as glucose and hypertension.
Unpublished Study Associates Testosterone With Greater Heart Risk
In August 2010, an unpublished report was circulated in the media that contradicted numerous published studies showing higher levels of testosterone protect against heart attack.53
This negative report was based on a study of less than 700 men (aged 65 and older) and claimed that men with higher testosterone doubled their risk of a heart attack or other cardiac events.
While even the author of this study admitted the findings were preliminary and had not been peer-reviewed, one striking discrepancy was that it defined high total testosterone as being greater than 495 ng/dL. Recall that in the much larger (2,416 men) published study (described at the beginning of this article) that a 30% reduction in cardiovascular events did not occur until total testosterone levels exceeded 550 ng/dL.
As is typical of so many of these studies, estrogen levels do not appear to have been measured, so we have no idea if any of these men in this negative study had the youthful balance of testosterone and estrogen required to protect against cardiovascular disease. (Estrogen was measured in the study showing reduction in cardiovascular events in men with thehighest testosterone level.)
How Testosterone Protects Against Heart Attacks
Most people know that higher blood levels of HDL protect against atherosclerosis and subsequent heart attack. What few understand is the critical role that testosterone plays in enabling HDL to remove built-up cholesterol from the arterial wall.
HDL removes cholesterol from the arterial wall and returns it to the liver for safe disposal via a process known as reverse cholesterol transport. Testosterone enhances HDL-induced reverse cholesterol transport from the arterial wall.9 That is one of testosterone’s unique and lifesaving anti-atherosclerotic effects.
While a person can reduce their arterial wall exposure to cholesterol through healthier diets and by taking certain drugs, the average person still synthesizes about 750 mg every day of cholesterol in their peripheral tissues (outside of the liver). If there is any distortion in the HDL-mediated removal of cholesterol (i.e. reverse cholesterol transport) from the arterial wall, the consequence is atherosclerosis.54
Said differently, testosterone is required for optimal transport of excess cholesterol from our tissues and blood vessels to our liver for processing and disposal. In the testosterone-deficient state, reverse cholesterol transport is compromised, and excess cholesterol cannot be removed from the arterial wall.55-57
HDL and testosterone levels often plummet in aging humans.59,60 The combination of low HDL and low testosterone virtually guarantees an explosion in demand for vascular stents and drugs that earn tens of billions of dollars in profits each year for pharmaceutical behemoths.
Under optimal circumstances, HDL efficiently removes cholesterol from arterial walls and then transports it (via reverse cholesterol transport) to the liver for elimination (mostly through the bile duct into the intestines). When there is a deficiency of testosterone, HDL is less efficient in removing debris from the arterial wall and the liver is less efficient in breaking down cholesterol- laden HDL from the blood- stream.
Armed with this knowledge, you can now see past the charade perpetrated by the medical establishment that still questions the value of testosterone supplementation.
Numerous well-controlled human studies show that higher testosterone levels play a critical role in maintaining healthy blood flow throughout the body by accelerating reverse cholesterol transport—thereby helping to prevent atherosclerosis.61,62
CHART 1. HOW TESTOSTERONE AFFECTS HDL
- Testosterone elevates the hepatic lipase enzyme that the liver needs to safely clear the body of excess cholesterol.
- The liver contains a receptor called scavenger receptor B1 that acts to stimulate cholesterol uptake for processing and disposal. Testosterone beneficially increases scavenger receptor B1.9
- Furthermore, a liver enzyme called hepatic lipase functions to remove phospholipids from the surface of HDL and helps enhance the uptake of these HDL-derived lipids by scavenger receptor B1.9,10,58
- Testosterone increases the activity of hepatic lipase.10
- By increasing both scavenger receptor B1 and hepatic lipase activities, testosterone facilitates an increase in reverse cholesterol transport, a process that removes excess cholesterol from the tissues and carries it to the liver for processing and disposal.9,10
- The important take home point is the critical role of reverse cholesterol transport in enabling HDL to protect against atherosclerosis.
Low Testosterone Sharply Increases Coronary Artery Disease Risk
The relationship between low testosterone and increased coronary artery disease incidence has been the featured topic of several covers of Life Extension Magazine® over the past two decades.
One study evaluated men under age 45 who presented with coronary artery disease compared with an age-matched control group. The findings revealed that even moderately reduced free testosterone blood levels (below 17.3 pg/mL of blood) in these younger men resulted in a 3.3-fold greater risk of developing premature coronary artery disease compared with men who had values above 17.3 pg/mL.70
To put this testosterone blood reading in perspective, aging men who don’t use testosterone-boosting nutrients or drugs often have very low free testosterone blood levels (less than 10 pg/mL of blood). These same men often have low HDL blood test readings in the danger zone (less than 40-50 mg/dL).
More recent studies confirm low blood levels of free testosterone increase cardiovascular mortality in men.71,72
Is it any wonder that despite aggressive use of statin drugs and other advances in cardiac medicine, heart attack and stroke are still today’s leading killers?
Testosterone for Chronic Heart Failure
Chronic heart failure is a disabling condition characterized by exercise intolerance and shortness of breath. The disease arises from prolonged inflammatory cytokine activation that also causes severe muscle wasting. Testosterone increases anabolic function, improves arterial dilation, augments cardiac output, and is known to have anti-inflammatory activities. Low testosterone is a common characteristic in men suffering from heart failure.
In an interesting report, 20 men with an average age of 62 took part in a randomized study in which testosterone or placebo was injected every two weeks for 12 weeks. Compared to the placebo group, men receiving testosterone could walk 3.5 times farther.73 Mean symptom scores and a critical blood measurement of heart function (brain natriuretic peptide) improved in men receiving testosterone, but not in the placebo group.
A trend toward improved mood scores was noted in the testosterone group, which is important because men with chronic heart failure have high rates of depression. The doctors concluded that 12 weeks of testosterone treatment led to significant improvements in physical capacity and symptoms.73
CHART 2. NATURAL HORMONES SLASH HEART DISEASE MORTALITY!
A landmark study analyzed the relationship of natural hormones (free testosterone, DHEA, and insulin-like growth factor-1 [IGF-1]) to death rates in men suffering from chronic heart failure.63 The findings from this study are tabulated on the chart in this box. As one can see, more men die when any of these hormones are deficient. This same chart shows catastrophic mortality when two or more of these hormones are deficient.63
A large number of studies reveal that higher testosterone or dehydroepiandrosterone (DHEA) levels are associated with reduced heart disease risk.64-69 DHEA is a low-cost dietary supplement, while IGF-boosting nutrients and natural testosterone cream are available to Americans at affordable prices.
Cardiac drugs generate outrageous profits for pharmaceutical interests. Pharmaceutical companies thus face huge economic losses if too many Americans use natural hormones to reduce their reliance on expensive prescription drugs.
Testosterone and Stroke Risk
One way to evaluate one’s risk for a stroke is to undergo an ultrasound test to measure carotid artery thickness. When excess occlusion is detected, a risky surgical procedure (carotid endarterectomy) is performed to restore blood flow to the brain.
In a study published by the American Heart Association in April 2004, ultrasounds were used to measure the carotid intima-media thickness in 195 independently living elderly men in 1996 and again in 2000. The researchers also measured blood levels of free testosterone in these men.
The results showed that men with low testosterone had a 3.57 times greater progression of carotid intima-media thickening than those with higher testosterone levels. These associations were independent of body mass index, waist-to-hip ratio, hypertension, diabetes, smoking, and serum cholesterol levels. The doctors concluded:
“Low free testosterone levels were related to intima-media thickening of the common carotid artery in elderly men independently of cardiovascular risk factors.” 21
Doctors Overlook Lethal Impact of Estrogen Imbalance
When Life Extension® started offering comprehensive blood test panels back in 1996, men did not understand why we were checking their estrogen levels. Back in those days, estrogen was considered a hormone of importance only to women.
We tested estrogen based on published data indicating that when estrogen levels are unbalanced, the risk of degenerative disease in aging men skyrockets.38,47-52 Of concern to us 16 years ago were reports showing that excess estrogen contributes to the development of atherosclerosis.74,75 Human clinical studies conducted more than a decade later confirmed our suspicions. Men with even slightly elevated estrogen levels doubled their risk of stroke and had far higher incidences ofcoronary artery disease.43,76,77 Our early observations also revealed that men presenting with benign prostate enlargement or prostate cancer had higher blood estrogen levels (and often low free testosterone blood levels).78-81Subsequent clinical studies help confirm our early observations.82-86
Insufficient estrogen, on the other hand, predisposes men to osteoporosis and bone fracture.87,88
The fact that 99% of men today have no idea what their blood estrogen levels are helps explain the epidemic of age-related disease that is bankrupting this nation’s medical system.
A study published in the Journal of the American Medical Association (JAMA) measured blood estradiol (a dominant estrogen) in 501 men with chronic heart failure. Compared to men in the balanced estrogen quintile, men in the lowest estradiol quintile were 217% more likely to die during a 3-year follow-up, while men in the highest estradiol quintile were133% more likely to die.39
The men in the balanced quintile—with the fewest deaths—had serum estradiol levels between 21.80 and 30.11 pg/mL. This is virtually the ideal range that Life Extension has long recommended male members strive for.
The men in the highest quintile who suffered 133% increased death rates had serum estradiol levels of 37.40 pg/mL or above. The lowest estradiol group that suffered a 217% increased death rate had serum estradiol levels under 12.90 pg/mL.
The dramatic increase in mortality in men with unbalanced estrogen (i.e., estradiol levels either too high or too low) is nothing short of astounding. It uncovers a gaping hole in conventional cardiology practice that is easily correctable and explains why clinical trials on aging men that fail to measure estradiol have serious shortcomings.
This study revealing the lethal dangers of estrogen imbalance was published in conventional medicine’s Bastille of knowledge—the Journal of the American Medical Association, yet doctors continue to design clinical trials on aging men that measure total and/or free testosterone levels, but fail to account for estradiol, which can sharply increase when large doses of testosterone are administered.
Low Testosterone Increases Prostate Cancer Risk
Fear of prostate cancer is the leading reason why aging men have shied away from restoring their free testosterone to youthful ranges. To dispel this concern, Life Extensionlong ago analyzed every published study and found there is no basis for asserting that testosterone causes prostate cancer.89-94
Our observations from the thousands of blood tests we perform each year for members confirm this. What we found is that men with low testosterone appear to be more likely to contract prostate cancer.
In the landmark book, Testosterone for Life (McGraw-Hill, 2008), Harvard professor Abraham Morgentaler thoroughly discredited the notion that testosterone causes prostate cancer.95
What came as a bombshell to the medical establishment was the compilation by Dr. Morgentaler of scientific facts showing that men with low testosterone levels have an increased percentage of prostate cancer-positive biopsies.96,97
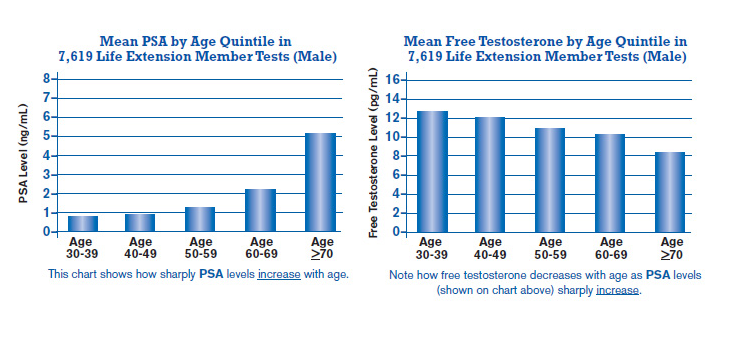
To further help dispel the myth that higher testosterone levels increase PSA levels (and presumably prostate cancer risk), the two charts (on the next page) compiled from our blood test analysis clearly show that as free testosterone levels decline in aging men, their PSA levels sharply increase.
What are Optimal Free Testosterone Levels?
The number of men who suffer testosterone deficiency is so high that laboratory reference ranges accept ridiculously low levels as “normal.”
We at Life Extension suggest that men maintain their free testosterone in the range of 20 to 25 pg/mL of blood.98
Conventional blood labs, on the other hand, say aging men are alright with as little as 6.6 pg/mL of free testosterone in their blood—an absurdly low level! (THAT IS WHAT THE AUSTRALIAN GOVERNMENT HAS DECIDED BECAUSE OF APPALLING ADVICE FROM IGNORANT UNEDUCATED EXPERTS!!!)
Mainstream medicine’s ignorance regarding the need to maintain free testosterone in the higher ranges is a significant cause of premature disability and death in aging men.
When Life Extension conducted a study of its members free testosterone blood levels two years ago, a startling 86% of the men had less than 15 pg/mL of free testosterone, placing them at high risk for virtually every age-related disease.
Free testosterone is the biologically active form of this hormone measured in the blood. When looking at total testosterone
blood levels, one should strive for a moderately youthful range of 700-900 ng/dL, though conventional reference ranges state that levels as low as 193 ng/dL are sufficient, a range that we at Life Extension believe is woefully inadequate.
Low Estradiol and Testosterone Predict Mortality in Aging Men
Sales of testosterone replacement drugs have surged more than 20-fold in response to studies linking low testosterone to a host of common maladies.
In a study of 3,014 men aged 69-80 years, serum levels of testosterone and estradiol were measured during a mean follow-up of 4.5 years. Men with low testosterone had 65% greater all-cause mortality, while men with low estradiol suffered 54% more deaths.40
Those men low in estradiol and testosterone were almost twice as likely to die (a 96% increase in mortality) compared to men in the optimal ranges.40
This large study of aged men corroborates prior published reports linking imbalances of testosterone and/or estradiol with greater incidences of degenerative disease and death.6,7,13-18
How Do Men Naturally Make Estrogen?
Women synthesize most of their estrogen in their ovaries and other reproductive tissues.
Since men lack this female anatomy, they need to produce estrogen through a process involving an enzyme called aromatase that transforms testosterone into estradiol.
Aging men sometimes have too much aromatase activity, which causes their testosterone to convert to excess estradiol. This results in depletion of vital testosterone while spiking estradiol to unsafe ranges.
Some men lack aromatase and suffer an estrogen deficit. Other men produce so little endogenous testosterone that there is not enough to convert into estrogen, which causes low levels of both free testosterone and estradiol.
Fortunately, no matter what the underlying cause, aging men can easily achieve optimal free testosterone and estradiol serum levels.
Free testosterone is the unbound form that is biologically available to cell receptor sites throughout the body. Measuring free testosterone blood levels is the most accurate way of assessing testosterone status in aging men.
How Aging Men Can Control Their Estrogen Levels
An epidemic problem we at Life Extension observe in aging male members is insufficient free testosterone, i.e., less than 15-20 pg/mL of serum. When accompanied by excess estradiol (over 30 pg/mL of serum), this can signal excess aromatase enzyme activity.
Excess aromatase robs men of their testosterone while exposing them to higher than desirable estradiol.99 Aromatase can be suppressed with absorbable forms of chrysin (a plant flavonoid) and/or lignans such as those extracted from the Norway spruce tree (HMRlignan™).100-104
If these nutrients fail to reduce estradiol adequately, then we suggest that men ask their doctor to prescribe a low-cost generic aromatase-inhibiting drug like anastrolzole in doses as low as 0.5 mg twice a week.
When aromatase is properly suppressed, estradiol levels are reduced to safe ranges, while free testosterone often increases, since less testosterone is being aromatized into estradiol.
Why Some Men Need Topical Testosterone Creams
Most testosterone in a man’s body emanates from the testes. Aging results in a decline in testicular output, thus necessitating the topical application of a testosterone cream to restore this vital hormone to youthful levels. Ideal free serum testosterone levels for most aging men are between 20-25 pg/mL.
As you may surmise, a man who produces too little testosterone risks a lethal deficiency of both free testosterone and estradiol. That’s because men need testosterone to synthesize estradiol in their bodies. In the presence of insufficient testosterone production, some aging men are vulnerable to low free testosterone and low estradiol that according to the latest study almost doubles their risk of dying over a 4.5 year period!40
Testosterone Decline and Aging
Aging is accompanied by reduced levels of hormones required to sustain life.
As testosterone levels decline in men, their risk of dying markedly increases.105-107
Heart disease,7,19,63,73,108 osteoporosis,109-111 and muscle wasting112-114 are strongly linked to testosterone deficiency, as are chronic inflammatory 13,115and neurodegenerative disorders.18,116 Most doctors are surprised to learn that men with low testosterone show an increased incidence of prostate cancer.117-121
Long before life prematurely ends, testosterone deficit can manifest in the form of psychological disturbances such asdepression,122-125 reduced sexual desire,126-129 and a loss of sense of well-being.125,130
The encouraging news is that restoring testosterone to youthful ranges can easily be accomplished at minimal cost.
THE MOST RECENT STUDY ON TESTOSTERONE AND VITAMIN D BLOOD LEVELS
As this article was being finalized, the findings from a brand new study were released that measured free testosteroneand 25-hydroxyvitamin D blood levels in a large group (2,069) men who were referred for coronary angiography.131 The results were nothing short of startling for those who fail to maintain optimal blood ranges of vitamin D and testosterone.
The researchers conducting this study carefully adjusted for confounding factors like age, body-mass-index, active smoking, physical activity, diabetes, C-reactive protein, prevalent coronary artery disease, serum calcium, and parathyroid hormone.
After study researchers corrected for these confounding factors, they found that in comparison with people having higher levels of 25-hydroxy- vitamin D and free testosterone in the body:
- Deficiencies of either free testosterone or 25-hydroxyvitaimin D resulted in a 40% increased risk for all-cause mortality (p=0.002);
- Deficiencies of free testosterone and 25-hydroxyvitaimin D resulted in a 111% increased risk for all-cause mortality (p<0.001).
- Deficiencies of free testosterone and 25-hydroxyvitaimin D resulted in a 77% increased risk forcardiovascular mortality (p<0.001);
- Deficiencies of either free testosterone or 25-hydroxyvitaimin D resulted in a 60% increased risk for non-cardiovascular mortality (p=0.011);
- Deficiencies of free testosterone and 25-hydroxyvitaimin D resulted in a 133% increased risk for non-cardiovascular mortality (p<0.001).
These sharp increases in mortality in response to deficiencies of testosterone and/or vitamin D reveal how far behind mainstream cardiologists are in treating patients with coronary artery disease. This study makes it abundantly clear that aging men should strive to achieve optimal blood levels of vitamin D and free testosterone, something that many Life Extension male members have been doing for the past three decades.
Critical Importance of Blood Testing
Today’s conventional physicians prescribe blood tests to check glucose, cholesterol, and triglycerides, but rarely check their male patients’ free testosterone and estradiol levels.
When looking at the horrifically high mortality rates associated with imbalances of these critical hormones, it becomes strikingly apparent that a significant number of heart attacks, strokes, bone fractures, and other degenerative diseases are easily preventable.
One reason these hormone blood tests are not normally prescribed is their high retail cost, and the fact that many insurance companies refuse to pay for them.
As a member of the Life Extension Foundation®, you don’t have to be victimized by conventional medical ignorance, high prices, or insurance company indifference.
Take Charge of Your Health with Low-Cost Blood Testing
An all-inclusive blood test panel that includes free testosterone and estradiol can retail for $1,000 at commercial labs. Life Extension members can obtain these same tests for only$199 during the Blood Test Super Sale.
If your blood test result reveals an imbalance of free testosterone and/or estradiol, you are in a position to initiate immediate corrective action. Not only can restoring youthful hormone balance save your life, but men (and women) often experience an enhancement in their quality of life after their hormones are adjusted to optimal ranges.
A complete description of the Male and Female Panels can be found at the end of this article. As you’ll readily see, these panels contain many important tests (such as total and free testosterone, estradiol, homocysteine, C-reactive protein, and DHEA) that mainstream doctors seldom check for.
You’ll also see that we added the 25-hydroxyvitamin D test to the low-priced Male and Female Panels, so members can easily attain optimal vitamin D levels in their body.
When you order these tests, a requisition form is sent listing blood drawing stations in your local area. Appointments are usually not necessary, meaning you can have your blood drawn at your convenience.
To order a comprehensive Male and/or Female Blood Test Panel, just call 1-800-208-3444. It is the single most important step you can take to ensure your continued good health.
The Blood Test Super Sale ends June 4, 2012, so you should order your tests soon and have your blood drawn any time thereafter at your convenience.
For longer life,
William Faloon
References
1. Bhasin S, Parker RA, Sattler F, et al. Effects of testosterone supplementation on whole body and regional fat mass and distribution in human immunodeficiency virus-infected men with abdominal obesity. J Clin Endocrinol Metab. 2007 Mar;92(3):1049-57.
2. Chen RY, Wittert GA, Andrews GR. Relative androgen deficiency in relation to obesity and metabolic status in older men.Diabetes Obes Metab. 2006 Jul;8(4):429-35.
3. Abate N, Haffner SM, Garg A, Peshock RM, Grundy SM. Sex steroid hormones, upper body obesity, and insulin resistance. J Clin Endocrinol Metab. 2002 Oct;87(10):4522-7.
4. Boyanov MA, Boneva Z, Christov VG. Testosterone supplementation in men with type 2 diabetes, visceral obesity and partial androgen deficiency. Aging Male. 2003 Mar;6(1):1-7.
5. Grossmann M, Thomas MC, Panagiotopoulos S, et al. Low testosterone levels are common and associated with insulin resistance in men with diabetes. J Clin Endocrinol Metab. 2008 May;93(5):1834-40.
6. Traish AM, Saad F, Guay A. The dark side of testosterone deficiency: II. Type 2 diabetes and insulin resistance. J Androl. 2009 Jan-Feb;30(1):23-32.
7. Hak AE, Witteman JC, de Jong FH, et al. Low levels of endogenous androgens increase the risk of atherosclerosis in elderly men: the Rotterdam study. J Clin Endocrinol Metab. 2002 Aug;87(8):3632-9.
8. Jones RD, Nettleship JE, Kapoor D, Jones HT, Channer KS. Testosterone and atherosclerosis in aging men: purported association and clinical implications. Am J Cardiovasc Drugs. 2005 5(3):141-54.
9. Langer C, Gansz B, Goepfert C, et al. Testosterone up-regulates scavenger receptor BI and stimulates cholesterol efflux from macrophages. Biochem Biophys Res Commun. 2002 Sep 6;296(5):1051-7.
10. Herbst KL, Amory JK, Brunzell JD, Chansky HA, Bremner WJ. Testosterone administration to men increases hepatic lipase activity and decreases HDL and LDL size in 3 wk. Am J Physiol Endocrinol Metab. 2003 Jun;284(6):E1112-8.
11. ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Major outcomes in moderately hypercholesterolemic, hypertensive patients randomized to pravastatin vs usual care: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT-LLT). JAMA. 2002 Dec 18;288(23):2998-3007.
12. Cziraky MJ, Watson KE, Talbert RL. Targeting low HDL-cholesterol to decrease residual cardiovascular risk in the managed care setting. J Manag Care Pharm. 2008 Oct;14(8 Suppl):S3-28; quiz S30-1.
13. Tang YJ, Lee WJ, Chen YT, et al. Serum testosterone level and related metabolic factors in men over 70 years old. J Endocrinol Invest. 2007 Jun;30(6):451-8.
14. Laaksonen DE, Niskanen L, Punnonen K, et al. Sex hormones, inflammation and the metabolic syndrome: a population-based study. Eur J Endocrinol. 2003 Dec;149(6):601-8.
15. Cutolo M, Seriolo B, Villaggio B, Pizzorni C, Craviotto C, Sulli A. Androgens and estrogens modulate the immune and inflammatory responses in rheumatoid arthritis. Ann NY Acad Sci. 2002 Jun;966:131-42.
16. Moffat SD, Zonderman AB, Metter EJ, Blackman MR, Harman SM, Resnick SM. Longitudinal assessment of serum free testosterone concentration predicts memory performance and cognitive status in elderly men. J Clin Endocrinol Metab. 2002 Nov;87(11):5001-7.
17. Ohlsson C, Barrett-Connor E, Bhasin S, et al. High serum testosterone is associated with reduced risk of cardiovascular events in elderly men. J Am Coll Cardiol. 2011 Oct 11;58(16):1674-81.
18. Gouras GK, Xu H, Gross RS, et al. Testosterone reduces neuronal secretion of Alzheimer’s beta-amyloid peptides. Proc Natl Acad Sci USA. 2000 Feb 1;97(3):1202-5.
19. Hogervorst E, Combrinck M, Smith AD. Testosterone and gonadotropin levels in men with dementia. Neuro Endocrinol Lett. 2003 Jun;24(3-4):203-8.
20. Debing E, Peeters E, Duquet W, Poppe K, Velkeniers B, Van Den Branden P. Men with atherosclerotic stenosis of the carotid artery have lower testosterone levels compared with controls. Int Angiol. 2008 Apr;27(2):135-41.
21. Muller M, van den Beld AW, Bots ML, Grobbee DE, Lamberts SW, van der Schouw YT. Endogenous sex hormones and progression of carotid atherosclerosis in elderly men. Circulation. 2004 May 4;109(17):2074-9.
22. Khaw KT, Dowsett M, Folkerd E, et al. Endogenous testosterone and mortality due to all causes, cardiovascular disease, and cancer in men: European prospective investigation into cancer in Norfolk (EPIC-Norfolk) Prospective Population Study.Circulation. 2007 Dec 4;116(23):2694-701.
23. Altschule MD, Tillotson KJ. The use of testosterone in the treatment of depression. N Engl J Med. 1948 239:1036-8.
24. Almeida OP, Yeap BB, Hankey GJ, Jamrozik K, Flicker L. Low free testosterone concentration as a potentially treatable cause of depressive symptoms in older men. Arch Gen Psychiatry. 2008 Mar;65(3):283-9.
25. Cherrier MM, Plymate S, Mohan S, et al. Relationship between testosterone supplementation and insulin-like growth factor-I levels and cognition in healthy older men. Psychoneuroendocrinology. 2004 Jan;29(1):65-82.
26. Mårin P, Krotkiewski M, Björntorp P. Androgen treatment of middle-aged, obese men: effects on metabolism, muscle and adipose tissues. Eur J Med. 1992 Oct;1(6):329-36.
27. Snyder PJ, Peachey H, Hannoush P, et al. Effect of testosterone treatment on bone mineral density in men over 65 years of age. J Clin Endocrinol Metab. 1999 Jun;84(6):1966-72.
28. Kenny AM, Kleppinger A, Annis K, et al. Effects of transdermal testosterone on bone and muscle in older men with low bioavailable testosterone levels, low bone mass, and physical frailty. J Am Geriatr Soc. 2010 Jun;58(6):1134-43.
29. Malkin CJ, Pugh PJ, Morris PD, Asif S, Jones TH, Channer KS. Low serum testosterone and increased mortality in men with coronary heart isease. Heart. 2010 Nov;96(22):1821-5.
30. Ahlbom E, Prins GS, Ceccatelli S. Testosterone protects cerebellar granule cells from oxidative stress-induced cell death through a receptor mediated mechanism. Brain Res. 2001 Feb 23;892(2):255-62.
31. Pike CJ, Carroll JC, Rosario ER, Barron AM. Protective actions of sex steroid hormones in Alzheimer’s disease. Front Neuroendocrinol. 2009 Jul;30(2):239-58.
32. Hogervorst E, Bandelow S, Combrinck M, Smith AD. Low free testosterone is an independent risk factor for Alzheimer’s disease. Exp Gerontol. 2004 Nov-Dec;39(11-12):1633-9.
33. Ready RE, Friedman J, Grace J, Fernandez H. Testosterone deficiency and apathy in Parkinson’s disease: a pilot study. J Neurol Neurosurg Psychiatry. 2004 Sep;75(9):1323-6.
34. Boutron, I., Dutton, S., Ravaud, P., and D.G. Altman. 2010. Reporting and interpretation of randomized controlled trials with statistically nonsignificant results for primary outcomes. JAMA. 303(20): 2058-64.
35. Leape LL, Brennan TA, Laird N, et al. The nature of adverse events in hospitalized patients. Results of the Harvard Medical Practice Study II. N Engl J Med. 1991 324(6):377-84.
36. Available at: http://www.amcp.org/data/jmcp/CE_V7_61-68.pdf. Accessed Jan. 16, 2012.
37. Cohen PG. Obesity in men: the hypogonadal-estrogen receptor relationship and its effect on glucose homeostasis. Med Hypotheses. 2008 70(2):358-60.
38. Zumoff B. Hormonal abnormalities in obesity. Acta Med Scand Suppl. 1988 723:153-60.
39. Jankowska EA, Rozentryt P, Ponikowska B. Circulating estradiol and mortality in men with systolic chronic heart failure.JAMA. 2009 May 13;301(18):1892-901.
40. Tivesten A, Vandenput L, Labrie F, et al. Low serum testosterone and estradiol predict mortality in elderly men. J Clin Endocrinol Metab. 2009 Jul;94(7):2482-8.
41. Mohamad MJ, Mohammad MA, Karayyem M, Hairi A, Hader AA. Serum levels of sex hormones in men with acute myocardial infarction. Neuro Endocrinol Lett. 2007 Apr;28(2):182-6.
42. Cao J, Zou H, Zhu BP, et al. Sex hormones and androgen receptor: risk factors of coronary heart disease in elderly men.Chin Med Sci J. 2010 Mar;25(1):44-9.
43. Barud W, Palusinski R, Beltowski J, et al. Relation between markers of inflammation and estradiol in older men. Med Sci Monit. 2010 Dec;16(12):CR593-7.
44. Boyle JJ. Association of coronary plaque rupture and atherosclerotic inflammation. J Pathol. 1997 Jan;181(1):93-9.
45. Pugh PJ, Channer KS, Parry H, Downes T, Jone TH. Bio-available testosterone levels fall acutely following myocardial infarction in men: association with fibrinolytic factors. Endocr Res. 2002 Aug;28(3):161-73.
46. Basaria S, Coviello AD, Travison TG, et al. Adverse events associated with testosterone administration. N Engl J Med. 2010 Jul 8;363(2):109-22.
47. Suzuki K, Ito K, Ichinose Y, Kurokawa K, Suzuki T. Endocrine environment of benign prostatic hyperplasia prostate size and volume are correlated with serum estrogen concentration. Scand J Urol Nephrol. 1995 Mar;29(1):65-8.
48. Lindholm J, Eldrup E, Winkel P. Variability in plasma oestrogen concentrations in men with a myocardial Infarction. Dan Med Bull. 1990 Dec;37(6):552-6.
49. Usuki F, Nakazato O, Osame M, Igata A. Hyperestrogenemia in neuromuscular diseases. J Neurol Sci. 1989 Feb;89(2-3):189-97.
50. Small M, MacRury S, Beastall GH. Oestradiol levels in diabetic men with and without a previous myocardial infarction. Q J Med. 1987 Jul;64(243):617-23.
51. Phillips GB. Evidence for hyperestrogenemia as the link between diabetes mellitus and myocardial infarction. Am J Med. 1984 Jun;76(6):1041-8.
52. Klaiber EL, Broverman DM, Haffajee CI, Hochman JS, Sacks GM, Dalen JE. Serum estrogen levels in men with acute myocardial infarction. Am J Med. 1982 Dec;73(6):872-81.
53. Available at: http://www.webmd.com/heart-disease/news/20100622/high-testosterone-may-raise-heart-risk. Accessed March 19, 2012.
54. Assmann G, Nofer JR. Atheroprotective effects of high-density lipoproteins. Annu Rev Med. 2003 54:321-41.
55. Attia N, Nakbi A, Smaoui M, et al. Increased phospholipid transfer protein activity associated with the impaired cellular cholesterol efflux in type 2 diabetic subjects with coronary artery disease. Tohoku J Exp Med. 2007 Oct;213(2):129-37.
56. Wu FC, von Eckardstein A. Androgens and coronary artery disease. Endocr Rev. 2003 Apr;24(2):183-217.
57. Traish AM, Abdou R, Kypreos KE. Androgen deficiency and atherosclerosis: The lipid link. Vascul Pharmacol. 2009 Nov-Dec;51(5-6):303-13.
58. Cucuianu M, Coca M, Hancu N. Reverse cholesterol transport and atherosclerosis. A mini review. Rom J Intern Med. 2007 45(1):17-27.
59. Yeap BB, Almeida OP, Hyde Z, et al. In men older than 70 years, total testosterone remains stable while free testosterone declines with age. Eur J Endocrinol. 2007 May;156(5):585-94.
60. Wilson PW, Anderson KM, Harris T, Kannel WB, Castelli WP. Determinants of change in total cholesterol and HDL-C with age: the Framingham Study. J Gerontol. 1994 Nov;49(6):M252-7.
61. Eckardstein A, Wu FC. Testosterone and atherosclerosis. Growth Horm IGF Res. 2003 Aug;13 Suppl AS72-S84.
62. Nettleship JE, Jones TH, Channer KS, Jones RD. Physiological testosterone replacement therapy attenuates fatty streak formation and improves high-density lipoprotein cholesterol in the Tfm mouse: an effect that is independent of the classic androgen receptor. Circulation. 2007 Nov 20;116(21):2427-34.
63. Jankowska EA, Biel B, Majda J, et al. Anabolic deficiency in men with chronic heart failure: prevalence and detrimental impact on survival. Circulation. 2006 Oct 24;114(17):1829-37.
64. Kapoor D, Malkin CJ, Channer KS, Jones TH. Androgens, insulin resistance and vascular disease in men. Clin Endocrinol (Oxf). 2005 Sep;63(3):239-50.
65. Barrett-Connor E, Khaw KT, Yen SS. A prospective study of dehydroepiandrosterone sulfate, mortality, and cardiovascular disease. N Engl J Med. 1986 Dec 11;315(24):1519-24.
66. Moriyama Y, Yasue H, Yoshimura M, et al. The plasma levels of dehydroepiandrosterone sulfate are decreased in patients with chronic heart failure in proportion to the severity. J Clin Endocrinol Metab. 2000 May;85(5):1834-40.
67. Herrington DM. Dehydroepiandrosterone and coronary atherosclerosis. Ann NY Acad Sci. 1995 Dec 29;774:271-80.
68. Feldman HA, Johannes CB, Araujo AB, et al. Low dehydroepiandrosterone and ischemic heart disease in middle-aged men: prospective results from the Massachusetts Male Aging Study. Am J Epidemiol. 2001 Jan 1;153(1):79-89.
69. Thijs L, Fagard R, Forette F, Nawrot T, Staessen JA. Are low dehydroepiandrosterone sulphate levels predictive for cardiovascular diseases? A review of prospective and retrospective studies. Acta Cardiol. 2003 Oct;58(5):403-10.
70. Turhan S, Tulunay C, Gulec S, et al. The association between androgen levels and premature coronary artery disease in men. Coron Artery Dis. 2007 May;18(3):159-62.
71. Militaru C, Donoiu I, Dracea O, Ionescu DD. Serum testosterone and short-term mortality in men with acute myocardial infarction. Cardiol J. 2010 17(3):249-53.
72. Vikan T, Schirmer H, Njølstad I, Svartberg J. Endogenous sex hormones and the prospective association with cardiovascular disease and mortality in men: the Tromsø Study. Eur J Endocrinol. 2009 Sep;161(3):435-42.
73. Pugh PJ, Jones RD, West JN, Jones TH, Channer KS. Testosterone treatment for men with chronic heart failure. Heart. 2004 Apr;90(4):446-7.
74. Jeppesen LL, Jørgensen HS, Nakayama H, Raaschou HO, Olsen TS, Winther K. Decreased serum testosterone in men with acute ischemic stroke. Arterioscler Thromb Vasc Biol. 1996 Jun;16(6):749-54.
75. Phillips GB, Pinkernell BH, Jing TY. The association of hypotestosteronemia with coronary artery disease in men.Arterioscler Thromb. 1994 May;14(5):701-6.
76. Abbott RD, Launer LJ, Rodriguez BL, et al. Serum estradiol and risk of stroke in elderly men. Neurology. 2007 Feb 20;68(8):563-8.
77. Wranicz JK, Cygankiewicz I, Rosiak M, Kula P, Kareba W. The relationship between sex hormones and lipid profile in men with coronary artery disease. Int J Cardiol. 2005 May 11;101(1):105-10.
78. Krieg M, Nass R, Tunn S. Effect of aging on endogenous level of 5 alpha-dihydrotestosterone, testosterone, estradiol, and estrone in epithelium and stroma of normal and hyperplastic human prostate. J Clin Endocrinol Metab. 1993 Aug;77(2):375-81.
79. Gann PH, Hennekens CH, Longcope C, Verhoek-Oftedahl W, Grodstein F, Stampfer MJ. A prospective study of plasma hormone levels, nonhormonal factors, and development of benign prostatic hyperplasia. Prostate. 1995 Jan;26(1):40-9.
80. Shibata Y, Ito K, Suzuki K, et al. Changes in the endocrine environment of the human prostate transition zone with aging: simultaneous quantitative analysis of prostatic sex steroids and comparison with human prostatic histological composition.Prostate. 2000 Jan;42(1):45-55.
81. Prins GS, Huang L, Birch L, Pu Y. The role of estrogens in normal and abnormal development of the prostate gland. Ann N Y Acad Sci. 2006 Nov;1089:1-13.
82. Prins GS, Korach KS. The role of estrogens and estrogen receptors in normal prostate growth and disease. Steroids. 2008 Mar;73(3):233-44.
83. Matsuda T, Abe H, Suda K. Relation between benign prostatic hyperplasia and obesity and estrogen. Rinsho Byori. 2004 Apr;52(4):291-4.
84. Ho CK, Nanda J, Chapman KE, Habib FK. Oestrogen and benign prostatic hyperplasia: effects on stromal cell proliferation and local formation from androgen. J Endocrinol. 2008 Jun;197(3):483-91.
85. Singh PB, Matanhelia SS, Martin FL. A potential paradox in prostate adenocarcinoma progression: oestrogen as the initiating driver. Eur J Cancer. 2008 May;44(7):928-36.
86. Giton F, de la Taille A, Allory Y, et al. Estrone sulfate (E1S), a prognosis marker for tumor aggressiveness in prostate cancer (PCa). J Steroid Biochem Mol Biol. 2008 Mar;109(1-2):158-67.
87. Mellström D, Vandenput L, Mallmin H, et al. Older men with low serum estradiol and high serum SHBG have an increased risk of fractures. J Bone Miner Res. 2008 Oct;23(10):1552-60.
88. Pernow Y, Hauge EM, Linder K, Dahl E, Sääf M. Bone histomorphometry in male idiopathic osteoporosis. Calcif Tissue Int. 2009 Jun;84(6):430-8.
89. Miner MM, Seftel AD. Testosterone and ageing: what have we learned since the Institute of Medicine report and what lies ahead? Int J Clin Pract. 2007 Apr;61(4):622-32.
90. Tan RS, Salazar JA. Risks of testosterone replacement therapy in ageing men. Expert Opin Drug Saf. 2004 Nov;3(6):599-606.
91. Rhoden EL, Averbeck MA, Teloken PE. Androgen replacement in men under-going treatment for prostate cancer. J Sex Med. 2008 Sep;5(9):2202-8.
92. Morgentaler A. Testosterone replacement therapy and prostate cancer. Urol Clin North Am. 2007 Nov;34(4):555-63.
93. Raynaud JP. Prostate cancer risk in testosterone-treated men. J Steroid Biochem Mol Biol. 2006 Dec;102(1-5):261-6.
94. Gooren L. Androgen deficiency in the aging male: benefits and risks of androgen supplementation. J Steroid Biochem Mol Biol. 2003 Jun;85(2-5):349-55.
95. Morgentaler A. Testosterone for Life. McGraw-Hill; 2008.
96. Schatzl G, Madersbacher S, Thurridl T, et al. High-grade prostate cancer is associated with low serum testosterone levels.Prostate. 2001 Apr;47(1):52-8.
97. Hoffman MA, DeWolf WC, Morgentaler A. Is low serum free testosterone a marker for high grade prostate cancer? J Urol. 2000 Mar;163(3):824-7.
98. Faloon W. Physician’s guide: Using blood tests to safely induce weight loss. Life Extension Magazine. 2009 Jun;15(6):42-63.
99. Leder BZ, Rohrer JL, Rubin SD, Gallo J, Longcope C. Effects of aromatase inhibition in elderly men with low or borderline-low serum testosterone levels. J Clin Endocrinol Metab. 2004 Mar;89(3):1174-80.
100. Ta N, Walle T. Aromatase inhibition by bioavailable methylated flavones. J Steroid Biochem Mol Biol. 2007 Oct;107(1-2):127-9.
101. Campbell DR, Kurzer MS. Flavonoid inhibition of aromatase enzyme activity in human preadipocytes. J Steroid Biochem Mol Biol. 1993 Sep;46(3):381-8.
102. Kellis JT Jr, Vickery LE. Inhibition of human estrogen synthetase (aromatase) by flavones. Science. 1984 Sep 7;225(4666):1032-4.
103. Saarinen NM, Warri A, Makela SI, et al. Hydroxymatairesinol, a novel enterolactone precursor with antitumor properties from coniferous tree (Picea abies). Nutr Cancer. 2000 36(2):207-16.
104. Wang C, Makela T, Hase T, Adlercreutz H, Kurzer MS. Lignans and flavonoids inhibit aromatase enzyme in human preadipocytes. J Steroid Biochem Mol Biol. 1994 Aug;50(3-4):205-12.
105. Shores MM, Matsumoto AM, Sloan KL, Kivlahan DR. Low serum testosterone and mortality in male veterans. Arch Intern Med. 2006 Aug 14;166(15):1660-5.
106. Laughlin GA, Barrett-Connor E, Bergstrom J. Low serum testosterone and mortality in older men. J Clin Endocrinol Metab.2008 Jan;93(1):68-75.
107. Shores MM, Moceri VM, Gruenwals DA, et al. low testosterone is associated with decreased function and increased mortality risk: a preliminary study of men in a geriatric rehabilitation unit. J Am Geriatr Soc. 2004 52:2077-81.
108. English KM, Mandour O, Steeds RP, Diver MJ, Jones TH, Channer KS. Men with coronary artery disease have lower levels of androgens than men with normal coronary angiograms. Eur Heart J. 2000 Jun;21(11):890-4.
109. Tuck SP, Francis RM. Testosterone, bone and osteoporosis. Front Horm Res. 2009 37:123-32.
110. Arver S, Lehtihet M. Current guidelines for the diagnosis of testosterone deficiency. Front Horm Res. 2009 37:5-20.
111. Cawthon PM, Ensrud KE, Laughlin GA, et al. Sex hormones and frailty in older men: the osteoporotic fractures in men (MrOS) study. J Clin Endocrinol Metab. 2009 Oct;94(10):3806-15.
112. Kamel HK, Maas D, Duthie EH, Jr. Role of hormones in the pathogenesis and management of sarcopenia. Drugs Aging. 2002 19(11):865-77.
113. Marcell TJ, Harman SM, Urban RJ, et al. Comparison of GH, IGF-I, and testosterone with mRNA of receptors and myostatin in skeletal muscle in older men. Am J Physiol Endocrinol Metab. 2001 Dec;281(6):E1159-E64.
114. Bhasin S, Storer TW, Berman N, et al. Testosterone replacement increases fat-free mass and muscle size in hypogonadal men. J Clin Endocrinol Metab. 1997 Feb;82(2):407-13.
115. Maggio M, Basaria S, Ceda GP, et al. The relationship between testosterone and molecular markers of inflammation in older men. J Endocrinol Invest. 2005 28(11Suppl Proceedings):116-9.
116. Lu PH, Masterman DA, Mulnard R, et al. Effects of testosterone on cognition and mood in male patients with mild Alzheimer disease and healthy elderly men. Arch Neurol. 2006 Feb;63(2):177-85.
117. Morgentaler A, Rhoden EL. Prevalence of prostate cancer among hypogonadal men with prostate-specific antigen levels of 4.0 ng/mL or less. Urology. 2006 Dec;68(6):1263-7.
118. Banach-Petrosky W, Jessen WJ, Ouyang X, et al. Prolonged exposure to reduced levels of androgen accelerates prostate cancer progression in Nkx3.1; Pten mutant mice. Cancer Res. 2007 Oct 1;67(19):9089-96.
119. Hoffman MA, DeWolf WC, Morgentaler A. Is low serum free testosterone a marker for high grade prostate cancer? J Urol. 2000 Mar;163(3):824-7.
120. Rhoden EL, Morgentaler A. Testosterone replacement therapy in hypogonadal men at high risk for prostate cancer: results of 1 year of treatment in men with prostatic intraepithelial neoplasia. J Urol. 2003 Dec;170(6 Pt 1):2348-51.
121. Morgentaler A, Bruning CO 3rd, DeWolf WC. Occult prostate cancer in men with low serum testosterone levels. JAMA. 1996 Dec 18;276(23):1904-6.
122. Almeida OP, Yeap BB, Hankey GJ, Jamrozik K, Flicker L. Low free testosterone concentration as a potentially treatable cause of depressive symptoms in older men. Arch Gen Psychiatry. 2008 Mar;65(3):283-9.
123. Pope HG Jr, Cohane GH, Kanayama G, Siegel AJ, Hudson JI. Testosterone gel supplementation for men with refractory depression: a randomized, placebo-controlled trial. Am J Psychiatry. 2003 Jan;160(1):105-11.
124. Seidman SN, Rabkin JG. Testosterone replacement therapy for hypogonadal men with SSRI-refractory depression. J Affect Disord. 1998 Mar;48(2-3):157-61.
125. Barrett-Connor E, Von Mühlen DG, Kritz-Silverstein D. Bioavailable testosterone and depressed mood in older men: the Rancho Bernardo Study. J Clin Endocrinol Metab. 1999 Feb;84(2):573-7.
126. Saad F, Gooren LJ, Haider A, Yassin A. A dose-response study of testosterone on sexual dysfunction and features of the metabolic syndrome using testosterone gel and parenteral testosterone undecanoate. J Androl. 2008 Jan-Feb;29(1):102-5.
127. Wang C, Cunningham G, Dobs A, et al. Long-term testosterone gel (AndroGel) treatment maintains beneficial effects on sexual function and mood, lean and fat mass, and bone mineral density in hypogonadal men. J Clin Endocrinol Metab. 2004 May;89(5):2085-98.
128. Arver S, Dobs AS, Meikle AW, Allen RP, Sanders SW, Mazer NA. Improvement of sexual function in testosterone deficient men treated for 1 year with a permeation enhanced testosterone transdermal system. J Urol. 1996 May;155(5):1604-8.
129. Davidson JM, Camargo CA, Smith ER. Effects of androgen on sexual behavior in hypogonadal men. J Clin Endocrinol Metab. 1979 Jun;48(6):955-8.
130. Amore M. Partial androgen deficiency and neuropsychiatric symptoms in aging men. J Endocrinol Invest. 2005 28(11 Suppl Proceedings):49-54.
131. Lerchbaum E, Pilz S, Boehm BO, Grammer TB, Obermayer-Pietsch B, März W. Combination of low free testosterone and low vitamin D predicts mortality in older men referred for coronary angiography. Clin Endocrinol (Oxf). 2012 Feb 22. doi: 10.1111/j.1365-2265.2012.04371.x.
Life Extension Magazine June 2012
